If only migraine symptoms were limited to the pain of a bad headache!
Unfortunately, migraine is much more complicated than that with symptoms that extent far beyond mere pain. This is why people who don’t get migraine don’t understand.
A migraine attack can’t be measured by the onset and relief of pain.
Some of the factors others generally don’t take into consideration are the emotional side effects, which can put migraine sufferers on a downward spiral of interlinked negative feelings.
Fear
1Fear of the pain itself is common, but there are also fears associated to how others will react if their migraine condition becomes known. This can cause all kinds of difficulties with family, friends, employers and colleagues. Migraineurs fear losing their jobs if employers find out about their condition, and this prevents them requesting accommodations that could help them avoid pain. Even receiving help from employers can provoke fear of causing resentment in colleagues, who may see such help as unwarranted special treatment.
On top of all this is a fear of the pain itself. Migraine is one of the four most disabling diseases in the world, according to the World Health Organization. Taking control of medication, understanding personal triggers, and being willing to discuss needs can help bring support and reduce fears.
Confusion
Cognitive disturbance is often part of a migraine variant called hemiplegicmigraine, but it can also affect others. Sufferers often find they can’t concentrate or form thoughts properly. These symptoms can make fear worse, as they’re often confused with stroke symptoms.
Guilt
The debilitating nature of migraine often means that sufferers are unable to cope with the dual demands of work and home, which puts extra pressure on partners and spouses who shoulder the burden of responsibility for childcare and household chores. Even when this burden is gracefully accepted, feelings of guilt can be crushing. Migraine sufferers find themselves constantly apologizing, which leads to other emotional disturbances since it makes them feel they are always in the wrong and to blame for their condition.
Repeated apology can provoke marital difficulties, as partners become irritated by the constant need to give reassurance. The result is a vicious cycle that is hard to break and sufferers need to find a way to stop blaming themselves. Speaking with doctors and therapists can help teach the whole family how to live with migraine.
Frustration and Anger
Chronic migraine limits lives. It cuts short careers, prevents enjoyment of a social life or hobby, causes missed family milestones such as children’s birthdays or important school events, all of which can lead to intense frustration and anger. Migraine sufferers often feel there is no point in making plans or accepting social invitations.
Constantly feeling frustrated and angry piles on the stress that, of course, increases the frequency and severity of migraine attacks, which in turn increases frustration and anger. Learning coping strategies that allow for planning and a more normal lifestyle can help reduce negative feelings. These could include arriving or leaving social event early, and finding ways to avoid personal triggers in noisy or crowded situations.
Resentment
Resentment can come at migraine sufferers from all angles. They resent the pain, resent the ways in which it limits their lives, and even find themselves resenting the good health of family members or close friends. Deep resentment leads to anger and frustration, irritability and mood swings. It breaks friendships, ruins relationships and makes feelings of guilt run deeper.
Depression
Medically, depression and migraine share common ground. The same neurotransmitter abnormalities are found in both migraine sufferers and those with clinical depression. Studies have found that people with migraine are 3.2 times more likely to suffer from depression, which leads to many other symptoms such as lack of self confidence, low self esteem and weight gain. Similar drugs used to treat depression are often prescribed for migraine, such as Sumatriptan or beta blockers. Speaking with care providers can help reduce feelings of depression and break the downward spiral.
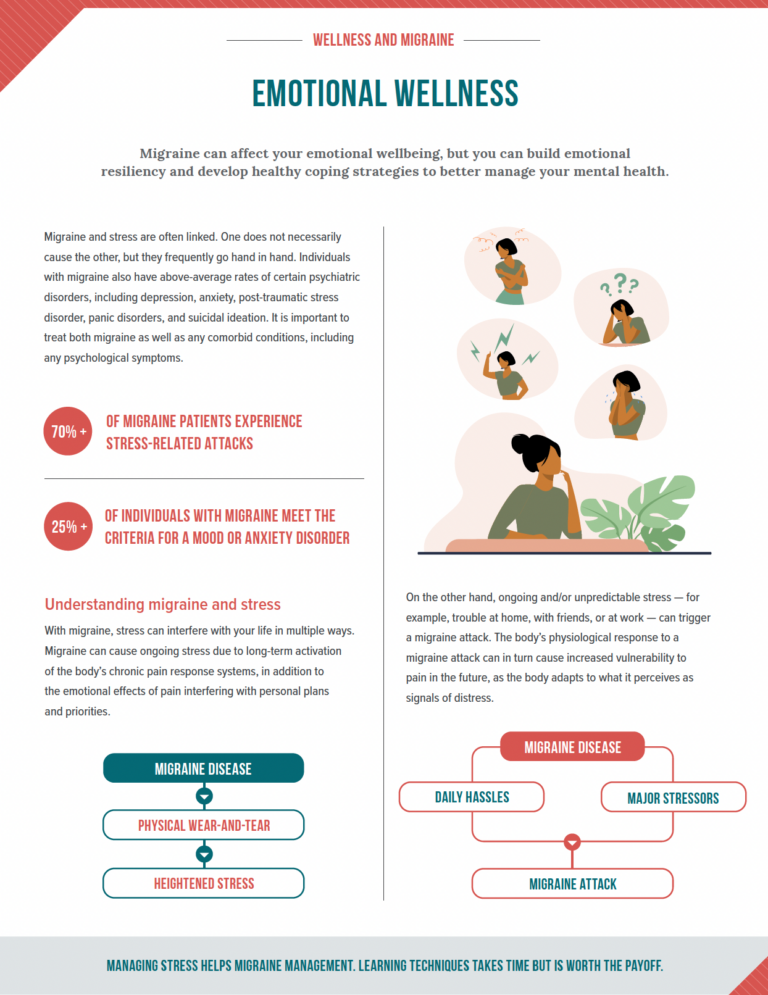
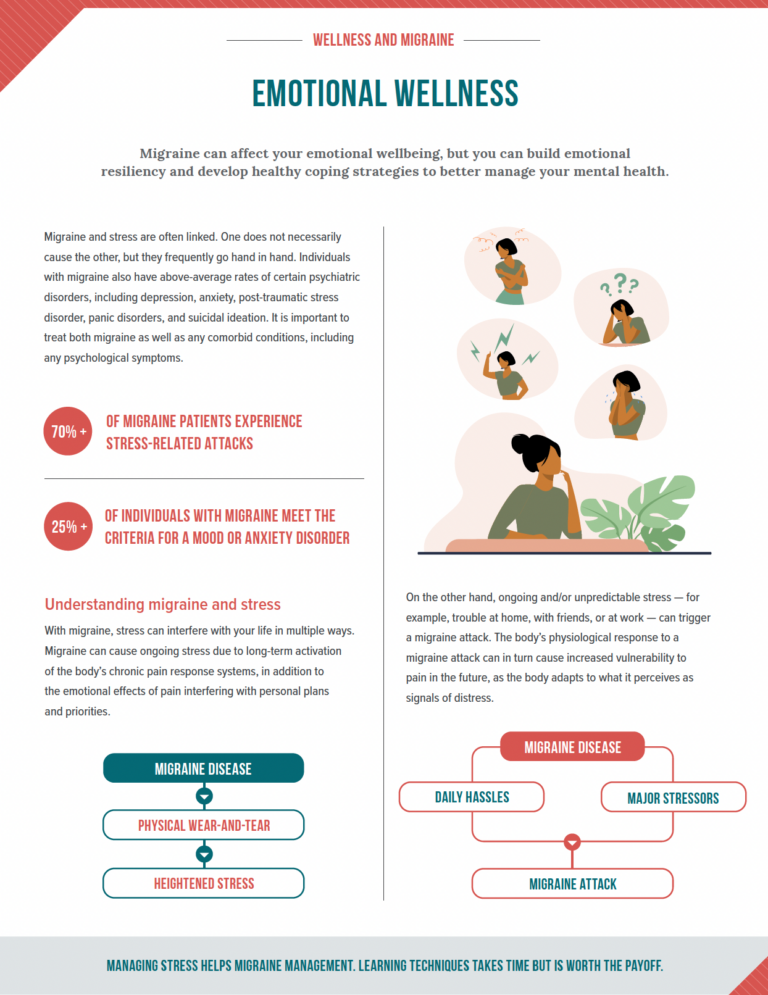
Stress
Stress comes from many different directions, including happy events such as weddings and birthday parties, even though we tend to think of stress as caused only by worrying situations.
All stress causes a similar reaction in the brain, which leads to dilation of blood vessels and muscle tension as the body prepares for flight or fight. Migraine pain can strike either during stress or afterwards in the letdown period. Stress management and relaxation techniques can help patients stay calm during stressful times, reducing the physical effects that often lead to pain.
Cognitive therapy that helps migraine sufferers cope with emotional side effects is often recommended over more medication. Sometimes called talk therapy, studies have shown it has a positive effect on emotions, teaching skills that empower migraineurs to manage their emotional responses.
If you’re struggling to cope with mood swings or other negative emotions due to migraine, don’t suffer in silence. Helping you to deal with those should be part of your migraine treatment.
Coping strategies are critical for people with chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME), as they usually feel as if their lives have been turned upside down. If you have CFS/ME, you may have lost your ability to work, participate in physical activities and socialize, as you did in the past. You may encounter disbelief from health professionals, and possibly family and friends, who suggest that you are not really sick because you “look fine.” Some people with CFS/ME start to believe this and berate themselves for “not doing enough,” which can lead to over-activity and “crashing.” Developing coping skills and getting emotional support are, therefore, a crucial part of healing.
A survey of people with CFS/ME in the US found that the most helpful skill for coping with the illness was “attitudinal adjustment.” The study participants also noted the importance of rest, pacing themselves, limiting their activities, minimizing their stress, reprioritizing their goals, educating themselves, and improving their diet and nutrition.
“Attitudinal adjustment” boils down to accepting the illness and taking care of yourself. Study participants made the following comments:
I stopped comparing myself to others.
I don’t waste time thinking about what life was like before I was sick.
I remind myself to be in the moment – that’s all there is.
I look back and compare myself to what I was like when I was first sick and appreciate the progress I have made so far.
A long-time survivor of CFS/ME and advocate said: ”The most important point that I want to make is that you are not your illness. You are still that funny, creative individual who just happens to have a chronic illness.”
Emotional and Spiritual Support
Anyone experiencing a chronic illness needs time to grieve the loss of their former life. Some people find that engaging in activities that cultivate their spiritual growth, such as prayer, yoga, religious services or meditation, is helpful.
Social Support
Isolation can be one of the most difficult aspects of having CFS/ME. Family and friends may not understand your lack of energy and what you are going through. This may be compounded by physicians and other health-care workers who refuse to see your illness as “real.”
The first step in helping others to understand your condition is to educate yourself, and then others. It can be helpful to connect with others who have the illness, for example, through a support group. Belonging to a group or community of people who understand and care can provide you with emotional support and useful information. Network with others who can support you, through brief telephone calls or emails.
Depression and Anxiety
Some people with CFS/ME feel depressed as a result of their illness, the many lifestyle changes and restrictions that they have had to cope with, such as being unable to participate in the activities they once enjoyed, as well as possible job, financial and relationship problems. If you have CFS/ME and think that you may be depressed, discuss this with your doctor. He or she may be able to refer you to a counsellor or support group.
Many people with CFS/ME experience anxiety. Relaxation techniques, pacing yourself and developing an attitude that can accommodate your situation will help. However, some individuals require medication to alleviate their anxiety or panic attacks.
Stress management tools may also help you deal with the depression and anxiety that can accompany chronic illness.
2Living with a chronic illness can make you feel angry, frustrated, down and even depressed. You will probably need some time to adjust to living with fibromyalgia. Know that you are not alone: fibromyalgia affects up to six percent of the population. Know too that many people with fibromyalgia lead rich and fulfilling lives.
Be patient. As you learn what goals are realistic for you and as you experiment with different treatment strategies, you will likely start to feel better.
Coping strategies are critical for people with fibromyalgia, as they usually feel as if their lives have been turned upside down. If you have fibromyalgia, you may have lost your ability to work, participate in physical activities and socialize, as you did in the past. Some people with fibromyalgia start to berate themselves for “not doing enough,” which can lead to over-activity and “crashing.” Developing coping skills and getting emotional support are, therefore, a crucial part of healing.
In addition to medications and physical therapies, relaxing regularly and limiting or weeding out your stress can help relieve your pain, as our minds and bodies are intricately connected.
You may want to try different relaxation techniques: deep breathing exercises, meditation, visualization techniques, progressive relaxation and biofeedback. As little as 20 minutes of relaxation a day can have health benefits, including reduced anxiety and an increased sense of well-being. Relaxation is particularly important after a period of activity (physical or mental), when you are feeling stressed, and before bedtime, to prepare for a good night’s sleep.
Choose a place in your house that will be your “relaxation space,” preferably a place where you can be alone, uninterrupted, for at least 10 minutes at a time. You may need to let your family know that this is a time when you want to be left alone.
Lie down on your bed or a comfortable couch and close your eyes. Take a few slow, deep breaths to settle in. Tell yourself that this is your time. When you feel settled, as you breathe in through your nose, say “re” silently to yourself, and then say “lax” as you exhale through your mouth.
An option is to also count to four as you inhale through your nose, pause, and then breathe out through your mouth for a count of four. It doesn’t matter how high you count, as long as you don’t force your breath. Try to do this for 10 minutes twice a day.
This breathing exercise can also be done at any time of day, for a few minutes, when you start to feel stressed. For example, if you are working and start to feel anxious, feel a headache coming on or a stiff neck, take a couple of minutes to do this relaxation exercise before you continue with your work. Do this as soon as you recognize your particular symptoms of stress. The earlier that you can break the stress-fatigue cycle with a relaxation technique, the better.
You can also do this simple exercise after you get into bed to help you fall asleep. It will help reduce worries that are interfering with your sleep. If you wake during the night with your mind racing, this exercise is also useful. As soon as you notice your thoughts returning to the “problem,” go back to your “re-lax” phrase and try to simply focus on your breath and the present moment, to still your mind and feel calmer.
Some people with fibromyalgia feel depressed as a result of their illness and the many lifestyle changes and restrictions that they may have had to cope with, such as being unable to participate in the activities they once enjoyed, as well as possible job, financial or relationship problems. If you have fibromyalgia and think that you may be depressed, talk to your doctor. He or she may be able to refer you to a counsellor or support group.
Many people with fibromyalgia experience anxiety. Relaxation techniques, pacing yourself and developing an attitude that can accommodate your situation will help. However, some individuals require medication to alleviate their anxiety or panic attacks.
Stress management tools may also help you deal with the depression and anxiety that can accompany chronic illness.
Social Support
Isolation can be one of the most difficult aspects of having fibromyalgia. Your friends, family and colleagues may not understand your pain and other symptoms, or what you are going through. Your sense of isolation may be compounded by health professionals who do not see your illness as “real” and may not be supportive.
The first step in helping others to understand your condition is to educate yourself, and then educate them. Explain how you’re feeling and be clear about what your limits are – what you can and cannot do at this time.
Many women find that joining a support group, to connect with others who have fibromyalgia, is helpful. Belonging to a community of people who understand and care can provide you with emotional support as well as useful information. You may want to include family and friends in the process and encourage them to air their feelings in a support group setting or with a counsellor. Network with others who support you, through brief telephone calls or emails.
Spiritual Support
Anyone experiencing a chronic illness needs time to grieve the loss of their former life.
Some women find that engaging in activities that cultivate their spiritual growth, such as prayer, yoga, religious services or meditation, is helpful.
Learning More About Your Condition: The more you learn about your condition and the more active you are in your own treatment, the more of a sense of control you will have.
3Emotional dysregulation is one of the more overlooked symptoms of ADHD, and one of the reasons people with ADHD are still misdiagnosed. Strong symptoms of emotional dysregulation can mimic other disorders like depression, bipolar, borderline personality, and even posttraumatic stress disorder (PTSD).1
What Is Emotional Dysregulation?
Emotional dysregulation is an impaired ability to control your emotional response, leading to extreme or overblown reactions that don’t really fit the situation. Some of the key signs and symptoms include:
- Emotional reactions that seem out of sync with their cause
- Difficulty calming down, even if you’re aware that you’re overreacting
- Low tolerance for frustration or annoyance
- Temperamental or prone to sudden outbursts
- Feeling completely overwhelmed by your emotions
- Difficulty refocusing your attention away from the emotion
It feels very “all or nothing” or “zero to 100” for me. Any negative trigger, ranging from finding out the grocery store is sold out of my preferred brand of bread to being turned down for a dream job, results in almost the same level of overwhelming disappointment.
It’s often hard to see past the emotion and get perspective: Is this thing really as important as I feel like it is? What’s a more rational response to this situation?
It’s even harder to move past it and convince my brain to focus on something else. The second my partner sets the salt shaker on the counter instead of putting it back by the spice rack, that’s all I can think about until it’s resolved.
Emotional Dysregulation Impacts Every Aspect of Life
For one of the least talked about aspects of ADHD, emotional dysregulation can also be the most disruptive.
At work, the ability to moderate your emotional response is a huge advantage in customer-facing positions as well as any role where you’re expected to work with a team. If you’re the “hypersensitive” or “temperamental” coworker, it can make your work life stressful and harm your ability to advance in your career.
In personal relationships, minor pet peeves (like the sound of chewing or the fact that your partner loads the dishwasher differently than you) can lead to explosive reactions that make your friends and loved ones feel like they have to walk on eggshells around you.
Psychologically, it can also lead to a lot of self-doubt and uncertainty surrounding your feelings. If your overreactions and impulses have burned you in the past, it can be hard to trust any of your emotions, even those more in line with the situation.
Why Is Emotional Dysregulation So Common in ADHD?
The science we have so far shows two main causes of emotional dysregulation in the ADHD brain: an overactive amygdala and an underactive frontal cortex.2
The amygdala is the part of the brain that triggers emotional responses so an overactive one is liable to trigger emotions that are stronger than they should be. Meanwhile, the frontal cortex is responsible for filtering and inhibiting those emotions so that you can react to a situation in a more adaptive and beneficial manner—like learning to hide your frustration and remain polite with an annoying customer to avoid escalating the situation into one that’s potentially even more frustrating.
If that cortex is underactive, it’s not inhibiting those emotional reactions as well as it could be. When you combine that with an amygdala that’s already generating emotions that are stronger than they need to be, it’s a recipe for impulsive behavior, explosive tempers, and hypersensitivity.
While science has shed some light on the parts of the brain responsible for emotional dysregulation, researchers still aren’t quite sure what part of the process is disrupted.
Emotional Regulation
The current model for emotional regulation breaks it down into five dimensions:
- Recognizing your own emotions
- Recognizing emotions in other people
- Emotional reactivity (your emotional threshold, or the level of intensity and duration of emotion that you’re able to tolerate without reacting to it)
- Arousal reduction (or the ability to calm yourself down)
- Emotional generation (or the ability to improve your mood)
A meta-analysis of 77 studies on emotional regulation in children with ADHD found that they had little problem recognizing emotions in themselves and others (the first two dimensions) and that those skills improved with age on par with children and young adults without ADHD.3
Where people with ADHD struggled the most was in emotional reactivity, which makes sense when you consider that an overactive amygdala is generating intense feelings that might exceed their emotional threshold more often than a normally functioning amygdala.
They also struggled with the fourth and fifth dimensions of emotional regulation: calming themselves down and intentionally changing their mood.
How to Develop and Practice Self-Regulation
How to Boost Your Emotional Regulation Skills
The neurological processes that seem to come naturally to those without ADHD may not work as well in an ADHD brain, but you can develop alternatives that function similarly and work with your brain with time and practice. Here are a few strategies you can try.
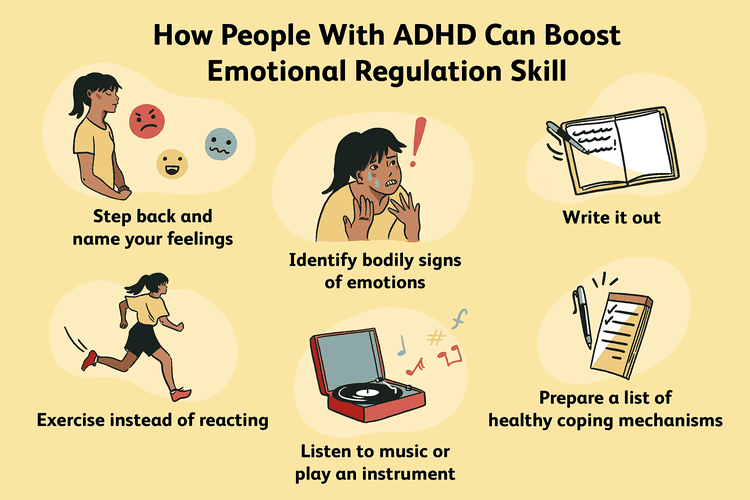
Step Back and Name Your Emotions
While people with ADHD don’t usually struggle with recognizing emotions, taking a break to acknowledge the feeling can be a first step toward regaining control. Before reacting or making any decision, do the following:
- Leave the situation. Go for a walk outside; go to the bathroom; get a glass of water, and stand in the backyard. If someone else is involved, say you need a few minutes to catch your breath and process.
- Identify all the bodily signs of your emotions. Is your heart racing? Is it hard to breathe? Are you sweating?
- Name the feeling. Anger? Shame? Sadness? Try to describe it as clearly and specifically as you can.
Because emotions can feel so overwhelming, and people with ADHD usually find challenges with calming down or talking themselves into a better mood, this exercise is a good compromise that can help dial down the intensity without relying on regulation skills you might not have.
It can help you detach a bit by putting you into the mode of analyzing the feeling rather than just being flooded by it.
Research has shown that naming your emotions, known as affective labeling, can reduce the intensity of negative emotions, possibly by increasing the intensity of positive ones.4
7 Things to Do if You Feel Emotional
Write It Out
For me, it often feels like the only way out is through. I can’t stop feeling an emotion, but I can see it through to the end without letting it do damage. To do that, I’ll usually write it out in a journal: explaining the situation, what triggered the emotion, what I’m feeling, and what my impulse or gut response is.
The process makes me feel like I’m expressing or acting on the feeling (which is what my brain wants to do) but in a way that won’t have long-term consequences. Then, once it feels less urgent, I can start thinking more clearly about an appropriate response.
If you’re angry, you’ll regret the mean things you said to someone you love after you calm down. If instead, you write those mean things down, you can let that feeling out without inflicting them on anyone. Then, tear it up or throw it away afterward.
Exercise Instead of React
The intensity of the emotion can give you this overwhelming urge to act, even if the rational part of your brain knows the emotion is wildly out of sync with the situation. Sometimes, you can channel that urge to take action into harmless exercise.
If a wave of emotion knocks you over, go for a run, lift weights or kick a punching bag. Physical exercise can use up that energy so that you don’t end up yelling at your partner or making impulsive decisions you’ll regret later.
For me, high-intensity exercises work the best (usually running as fast as I can) because it feels like the intensity of the activity matches the intensity of the emotion. But any physical movement can help, even if it’s just going for a walk or shooting hoops at a nearby basketball court.
Listen to Music (or Play an Instrument)
Studies confirm that people with ADHD experience improved moods after listening to music just like people without ADHD.5
You may struggle to intentionally change your mood on your own but music can help jumpstart the process. Make a playlist (or a few) with your favorite songs and listen to it whenever you’re struggling with an intense emotion.
As a bonus, research also shows playing a musical instrument is linked to improved emotional regulation in people with ADHD.6 So taking some music lessons can be a way to reduce symptoms of emotional dysregulation in the long term.
Make a List of Your Coping Mechanisms
What works in one situation might not work for another. If you’re at work, for example, you might not be able to just clock out and go for a spontaneous run around the block when a customer is getting on your nerves.
Prepare yourself for different situations by writing down a list of healthy coping mechanisms for a range of scenarios so that you have a quick reference to choose from whenever you find yourself suddenly flooded with emotion.
Emotional symptoms in Post Traumatic Stress Disorder and brain trauma can overlap, both involve mast cell activation and sensory overload. The emotional symptoms can be worsened by sleep disorders like sleep apnea which are over represented in these conditions 4 5. Where sleep apnea can be a cause of brain trauma if more severe, however with treatment can be reversed.
What causes emotional changes after TBI?6,7
- Emotional changes can occur if the TBI affects areas of the brain that control emotions. Changes to these brain regions and to the chemicals that help the brain work can affect how the person with TBI experiences or expresses emotion.
- People with TBI may have a hard time coping with their injury. They may need to adjust to a loss of independence, or to changes to their role in their family and in society. These changes can lead to frustration and dissatisfaction with their life.
- People with TBI may also have changes in their thinking abilities, such as memory, attention, speed of thinking, and reasoning. These changes can cause them to feel overwhelmed if they can’t remember things or keep up with what others are doing or saying. They may respond emotionally, with sadness, worry, or anger.
- Use of alcohol or other drugs can lead to emotional changes, and emotional distress may also lead to alcohol and drug use.
- People who had problems with depression or anxiety before the TBI may find that these problems are worse after the TBI. They may feel isolated, depressed, or misunderstood which can also affect emotions.
How to address emotional concerns after TBI
- Remember that emotional distress is not a sign of weakness and it is no one’s fault. A person can’t get over their distress by wishing it away or “toughening up.”
- Medicine and counseling or psychotherapy can help with emotional distress after TBI. Sometimes, a combination of both works best.
- If you choose to take medicine, you should work closely with the doctor or provider who prescribed the medication. Be sure to attend all follow-up visits about your medicine.
- If you choose counseling or psychotherapy, let your therapist know about your TBI. Ask them to help you write important concepts down so that you can review them at home. Tell your therapist if you need to have something repeated in order to understand it better.
- Stress and stressful situations can trigger emotional distress. People with TBI can take steps to reduce stress. For example, they can use relaxation techniques such as deep breathing or muscle relaxation, schedule breaks, and practice mindfulness activities.
- A daily schedule of structured activities and exercise can help reduce distress. Activities may include exercise, puzzles, or games.
- It is best to get treatment early to avoid needless suffering. Do not wait.
- If you (or your family member) have thoughts of suicide, get help.
Family members can help by changing the way they react to emotional distress after TBI:
- Remember that anxiety, depression, irritability, and other changes in emotion after TBI may be due to brain injury. Try not to take it personally. Also remember that changes in emotion are no one’s fault and try not to blame the person with TBI.
- Stay calm and try not to react in an emotional way yourself or to argue with the person with TBI. If you are angry or hurt, take a break before you talk to them.
- When they are acting out in anger, do not give in to their demands to try to calm them down. This can actually have the opposite effect of rewarding them for expressing their emotions in a non-helpful way. Resist the urge to give in to unreasonable demands. Instead, explain that you will talk to them when they are calm. Walk away and take a break until they are calmer.
- Provide feedback in a gentle and supportive way after the person is calm.
- Give the person with TBI opportunities to take a break to process their emotions. Encourage them to use deep breathing or listen to music to relax. Offer a quiet area, away from the stressor, to calm down and regain control. Then, redirect their attention to a different topic or activity.
- Give the person with TBI time to have structured independence and more control over his or her life.
- Tell them you recognize their emotions and want to understand their feelings and give the person with TBI a chance to talk about their feelings. People with TBI often have a hard time naming their emotions and might find it hard to recognize emotions in others. This means that they may not realize that they seem angry or that they are making others uncomfortable. You can help them identify their emotions and tell them how you feel.
- Seek out support. The family may benefit from social and professional support. Counseling can help relieve the family’s worry and help them to cope better each day.
RELATED FACTSHEETS
FACTSHEETS
Irritability, Anger, and Aggression After TBI
FACTSHEETS
FACTSHEETS
We function best at medium levels of stress. Deadlines and a small amount of pressure can bring out our best work.
But, too much stress for too long can make people feel overwhelmed. It can affect quality of life and cause problems with physical and mental health. It can also lead to behaviours that are harmful to our relationships with others.
Posttraumatic stress refers to a group of reactions that can occur after someone has experienced a traumatic event.
After facing a traumatic event, people often experience intense and difficult emotions. They feel tense and wound up, and these distressing emotions may continue even after the danger has passed. This can be exhausting. There are some practical techniques you can use when experiencing difficult emotions, including deep breathing and grounding.8 You can also benefit from managing stress and engaging in psychotherapy.
Dialectal Behavioural Therapy (DBT) may be recommended if you are finding it difficult to manage stress and are experience significant emotional dysregulation.
Managing stress
Some steps that might help you manage stress are:
- Understand your stress. It can be difficult to recognise that stress levels are building up. The stress scale tool can help you to monitor and ‘check in’ on how stressed you are feeling.Stress_scale_tool.pdf (205.68 KB)Monitoring helps increase awareness, so you can apply strategies to reduce your stress.
- Look at underlying causes. Identify and list the factors in your life that are causing your stress. Looking at the list with another person can help offer a different perspective.
- Identify things you can change. Underline the things you can change and make plans do so. Use our problem solving tool to help focus on one issue at a time.
- Adopt strategies for what you can’t change. One of the most effective ways to overcome stress is to change the way you respond to a stressful situation rather than trying to change the situation itself. Our challenge your thoughts tool can help you to think in more helpful and productive ways.
- Tell someone you trust. Let someone you trust know how you are feeling and what you need or want. Let them know what your limits are and try to remain respectful and calm. Staying positively connected to others is a critical stress management strategy.
- Practice relaxation. Learning relaxation techniques is a life skill which significantly helps to reduce stress and anxiety levels and improve life satisfaction and happiness.
- Look after yourself. Daily exercise and a healthy diet are extremely important. Our living well section has a range of suggestions and recipes for good health.
As trauma can reduce a persons window of tolerance (WOT) symptoms of emotional dysregulation may become an ongoing concern. This may be helped with dialectical behavioural therapy (DBT) or other forms of therapy.
- https://blog.themigrainereliefcenter.com/the-emotional-side-of-migraines ↩︎
- https://www.womenscollegehospital.ca/care-programs/environmental-health-clinic/fibromyalgia-syndrome/ ↩︎
- https://www.verywellmind.com/adhd-symptom-spotlight-emotional-dysregulation-5219946 ↩︎
- Sleep and PTSD https://www.ptsd.va.gov/publications/rq_docs/V27N4.pdf ↩︎
- https://sleepeducation.org/treating-sleep-apnea-reverses-brain-damage/#:~:text=OSA%20is%20a%20chronic%20disease,%2C%20difficulty%20concentrating%2C%20and%20moodiness. ↩︎
- dhttps://msktc.org/tbi/slideshows/emotional-problems-after-traumatic-brain-injury ↩︎
- https://msktc.org/tbi/tbi-topics/emotional-problems-after-tbi ↩︎
- https://www.phoenixaustralia.org/your-recovery/helping-yourself/ ↩︎
No Comments